With eClaims (also known as eTrans), which is the electronic claims service that is provided by Henry Schein One, you can submit dental and medical insurance claims electronically. Sending electronic claims through eClaims simplifies the complex and time-consuming task of sending insurance claims, allowing you to spend more time to interact with your patients. Electronic claims arrive at the insurance company faster than mailed claims, go directly into the insurance company's system, and are resolved faster than mailed claims, which results in your office receiving more timely payments. Electronic claims not only save time but materials and postage, so the cost of sending claims electronically is significantly lower than the cost of mailing printed claims.
Additionally, when sending electronic claims through eClaims, if a claim cannot be sent to the payor electronically, the claim will be printed and mailed for you, so you can send all your claims electronically even if some of your payors do not accept electronic claims.
Notes:
You can also submit an individual dental or medical insurance claim in Ledger.
To send electronic claims, you must register for eClaims, and the eTrans program (which is available as an add-on that you purchase separately) must be installed and configured on a computer with an Internet connection.
For information about setting up Dentrix Enterprise for billing medical insurance electronically, see the topic about the requirements for medical insurance claims.
Sending electronic claims and pre-treatment estimates if required attachments for any of the associated procedures are missing requires the "Eclaims: Require attachment, override" security right.
To submit electronic claims in Office Manager
To create and batch insurance claims, do any of the following as needed:
In Ledger, create dental or medical insurance claim, sending it directly to the Batch Processor.
Notes:
If you need to edit a dental or medical insurance claim after creating it, do so in Ledger, and then send (or resend) it to the Batch Processor.
You can create a secondary medical insurance claim only after you receive the adjudication on the primary medical insurance claim.
In Office Manager, create a batch of insurance claims, sending them to the Batch Processor.
In Office Manager, if you want to send specific claims, select them in the Batch Processor.
Do one of the following:
Click the Electronic Claim Submission button ![]() on the toolbar.
on the toolbar.
On the File menu, click ECS.
If applicable, do one of the following:
If the Password - Send Electronic Claims dialog box appears, user verification has been assigned to the "Send Electronic Claims" task. Do one of the following:
If your user account has been granted the "Send Electronic Claims" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Send Electronic Claims" security right, have a user with permission temporarily override this restriction so you can send claims this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Send Electronic Claims" security right. To have a user with permission temporarily override this restriction so you can send claims this one time, do the following:
On the message, click Yes.
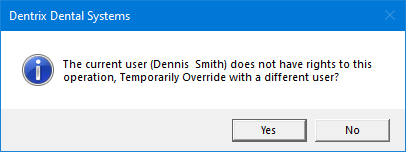
In the Password - Send Electronic Claims dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

The Electronic Claims Submission dialog box appears.

Set up the following options:
Select Claims to Submit - From the list, select one of the following options:
All Dental, Medical, and Institutional Claim Forms - To send all the dental claims and professional medical claims (as 837p files) in the Batch Processor that have an Unsent status (whether or not the claim format is electronic). Currently, sending institutional medical claims electronically as 837i files is not supported.
Selected Claim Forms - To send the selected claims in the Batch Processor that have an Unsent status (whether or not the claim format is electronic).
All Electronic Dental Claim Forms - To send all dental claims in the Batch Processor that have an electronic claim format and have an Unsent status.
All Electronic Medical Claim Forms - To send all professional medical claims (as 837p files) in the Batch Processor that have an electronic claim format and have an Unsent status. Currently, sending institutional medical claims electronically as 837i files is not supported.
All Dental Claim Forms - To send all dental claims in the Batch Processor that have an Unsent status (whether or not the claim format is electronic).
All Medical Claim Forms - To send all professional medical claims (as 837p files) in the Batch Processor that have an Unsent status (whether or not the claim format is electronic).
All Institutional Claim Forms - Currently, sending institutional medical claims electronically as 837i files is not supported.
Select Clinic/View - From the list, select one of the following options:
All Clinics - To send claims that are associated with all clinics for which your user account has been granted the "Send Electronic Claims" security right.
Current Clinic - To send claims that are associated with only the clinic that you are currently logged in to.
Current View - To send claims that are associated with the clinics for the current view and for which your user account has been granted the "Send Electronic Claims" security right.
To save the current settings for the next time that you send insurance claims electronically, select the Save as Default checkbox.
Click OK.
If any claims are skipped, a message appears as applicable to inform you that claims were skipped and the reasons why. Click OK to continue.
The following messages are possible:
A message may appear and state that you do not have permission to send claims from certain clinics. The number of claims that will not be sent appears.

A message may appear and state that certain claims are from a clinic that is not associated with a Data Service account. The number of claims that will not be sent appears.

Note: For each skipped claim, "Unsent" will appear in the Status column of the Batch Processor.
If a set of e-claims are being sent using multiple Data Service (eTrans) accounts, a message appears and states that the claims will be validated and sent in batches according to the Data Service account. Click OK to continue.

Note: If this message does appear, after you click OK, you must complete steps 10-18 for each account; otherwise, you will complete them only once.
If a claim or pre-treatment estimate has a procedure that requires an attachment for e-claims, but the claim does not have an attachment, the claim will not be sent. In this case, the Claim Review dialog box (or message box) appears. Do one of the following:
For multiple claims or pre-treatment estimates - In the Claim Review dialog box, click Send Remaining Claims. On the confirmation message that appears, click either Yes to send claims that are not listed, or No to return to the Claim Review dialog box.

Notes:
The Claim Sent date is blank if the claim was not sent previously.
The Procedure(s) requiring an attachment box contains a comma-delimited list of the procedure codes requiring an attachment. If there are duplicate procedures on the claim, the procedure appears only once.
Double-click a claim (not a pre-treatment estimate) to open the Claim Information window and add an attachment.
Right-click a claim or pre-treatment estimate, and then click one of the following options:
Go to Claim - To open the claim (or pre-treatment estimate) information.
Go to Ledger - To open the patient's Ledger.
Click Copy to Clipboard to copy all the data displayed, including the column headers, to the Windows Clipboard.
Clicking Close returns you to the Electronic Claims Submission dialog box.
For an individual claim or pre-treatment estimate - In the Claim Review message box, click OK.

The eClaims Pre-Submission Summary dialog box appears.

Note: eTrans performs a check on all of the claims you are sending, and each claim is given one of three statuses:
Validated - This status is assigned to claims that contain all the required information and are ready to be sent electronically.
Warning - This status is assigned to claims that are missing information (such as payor ID numbers, insurance plan numbers, and so forth). This status is also assigned to claims that require attachments (such as X-rays, panoramic films, periodontal charting information, and so forth). You can send claims with a Warning status to the insurance company (payor), but it is recommended that you correct the information on the claim before you send it.
Rejected - This status is assigned to claims that have an error that would cause the insurance company to reject the claim. If the error is caused by information included on the claim, delete the claim from both the Batch Processor and Ledger, correct the errors, recreate the claim, and re-send it to the Batch Processor for processing with your next batch of claims.
If there are any claims with a status of Warning or Rejected, to add missing information and/or edit incorrect information, do the following for each claim:
Click the link in the Status column.
The Edit Missing Claim Information dialog box appears.

Notes:
Add or edit the necessary information on each tab.
All options are required except for the second Street box on a given tab.
Changes you make in this dialog box are saved in Dentrix Enterprise.
On the Patient tab, set up the following options:
Date of Birth - The patient's birth date.
Address - Do one of the following:
Enter the patient's address.
To use the subscriber's address, select the Use Subscriber Address checkbox to populate the boxes with the claim subscriber's address.
Note: This checkbox is available only if all the required boxes of the Address are not populated, if the Use Patient Address checkbox is not selected on the Claim Subscriber or Other Subscriber tab, and if there is an address for the claim subscriber.

On the Claim Subscriber tab, set up the following options:
Date of Birth - The subscriber's birth date.
Subscriber ID # - The ID of the subscriber on the claim (primary or secondary, whichever appears).
Address - Do one of the following:
Enter the subscriber's address.
To use the patient's address, select the Use Patient Address checkbox to populate the boxes with the patient's address.
Note: This checkbox is available only if all the required boxes of the Address are not populated, if the Use Subscriber Address checkbox is not selected on the Patient tab, and if there is an address for the patient.

On the Providers tab, set up the following options:
Billing Provider - The billing provider's NPI, and the billing provider's TIN# or SS#.
Pay-To Provider - The pay-to provider's NPI, and the pay-to provider's TIN# or SS#.
Claim Rendering Provider - The claim rendering provider's NPI, and the claim rendering provider's TIN# or SS#.
Note: You do not need to enter dashes (-) for any of the numbers.

On the Insurance Plan tab, enter the Address where claims are sent for the insurance plan.

On the Other Subscriber tab - Set up the following options for the other subscriber (the secondary subscriber if this is a primary claim; or the primary subscriber if this is a secondary claim):
Date of Birth - The subscriber's birth date.
Subscriber ID # - The ID of the subscriber on the claim (primary or secondary, whichever appears).
Address - Do one of the following:
Enter the subscriber's address.
To use the patient's address, select the Use Patient Address checkbox to populate the boxes with the patient's address.
Note: This checkbox is available only if all the required boxes of the Address are not populated, if the Use Subscriber Address checkbox is not selected on the Patient tab, and if there is an address for the patient.

Click OK.
You are returned to the eClaims Pre-submission Summary dialog box.
Note: If additional electronic claims were sent to the Batch processor from another computer while you were editing a claim, those additional claims now appear in the eClaims Pre-submission Summary dialog box.
If you need to leave the eClaims Pre-submission Summary dialog box to make corrections, such as add missing attachments, to generate a report that you can refer to as you make those corrections, click Print Report. Click Cancel, make corrections, add attachments as needed, and then attempt to submit the claims again. The eClaims Pre-submission Summary dialog box appears again.
Note: If the Place of Service code or Service Facility TIN is missing on a medical insurance claim, you must fix the error in Ledger.
Again, check for claims with a status of Warning or Rejected, and make changes as needed.
Select the checkbox of each claim that you want to send electronically.
Notes:
Make sure that you carefully review the claims before submitting any of them.
By default, claims with a status of Validated or Warning are selected; claims with a status of Rejected are not.
Click Send Selected Claims.
If your eTrans account is locked by another user when you attempt to submit electronic claims, a message appears. Click one of the following options:
A here button within the new text "If you feel that the reported use of this eTrans UserId is inaccurate, you attempt to clear this lock by clicking here."
A Retry button to attempt to submit the claims again.
A Cancel button to dismiss the message and cancel the submission.

The Sending Claims dialog box appears and displays the progress of the submission.

Click OK on message that appears when the submission is successful.

You are returned to the Sending Claims dialog box.

Note: If you want to view a detailed log of the transmission, click Show Messages.

The expanded dialog box provides the following options for the log:
Copy to Clipboard - If you want to copy the output log to the Windows Clipboard so that you can paste it into another program, click Copy to Clipboard. (This is only necessary if there is a problem and a support representative needs the information for troubleshooting.)
Email - If you want to send a message containing the output log, click Email.
Click Finish.
After you send electronic claims, eTrans sends reports to the Batch Processor that you can view. These reports include the eClaims Pre-submission Summary Report and the Transmission Report. If any of the claims that you sent were rejected, the Error Report will open automatically. Review these reports to ensure that your claims are being processed and to view important information about the electronic claims you have sent and about your eTrans account.
Once the claims have been successfully transmitted, delete them from the Batch Processor.
Note: Deleting a claim from the Batch Processor does not delete the corresponding claim in Ledger.